MercoPress. South Atlantic News Agency
Widespread antibiotic resistance to bacterial infections confirmed in WHO global testing
 Resistance to penicillin, the medicine used for decades worldwide to treat pneumonia, ranged from zero to 51% among reporting countries
Resistance to penicillin, the medicine used for decades worldwide to treat pneumonia, ranged from zero to 51% among reporting countries 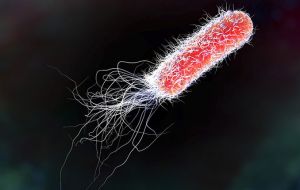 Between 8% to 65% of E. coli associated with urinary tract infections presented resistance to ciprofloxacin, an antibiotic commonly used to treat this condition.
Between 8% to 65% of E. coli associated with urinary tract infections presented resistance to ciprofloxacin, an antibiotic commonly used to treat this condition.  “The report confirms the serious situation of antibiotic resistance worldwide,” says Dr Marc Sprenger, director of WHO’s Antimicrobial Resistance Secretariat.
“The report confirms the serious situation of antibiotic resistance worldwide,” says Dr Marc Sprenger, director of WHO’s Antimicrobial Resistance Secretariat. WHO’s first release of surveillance data on antibiotic resistance reveals high levels of resistance to a number of serious bacterial infections in both high- and low-income countries. WHO’s new Global Antimicrobial Surveillance System (GLASS) reveals widespread occurrence of antibiotic resistance among 500 000 people with suspected bacterial infections across 22 countries.
The most commonly reported resistant bacteria were Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, and Streptococcus pneumoniae, followed by Salmonella spp. The system does not include data on resistance of Mycobacterium tuberculosis, which causes tuberculosis (TB), as WHO has been tracking it since 1994 and providing annual updates in the Global tuberculosis report.
Among patients with suspected bloodstream infection, the proportion that had bacteria resistant to at least one of the most commonly used antibiotics ranged tremendously between different countries – from zero to 82%. Resistance to penicillin – the medicine used for decades worldwide to treat pneumonia – ranged from zero to 51% among reporting countries. And between 8% to 65% of E. coli associated with urinary tract infections presented resistance to ciprofloxacin, an antibiotic commonly used to treat this condition.
“The report confirms the serious situation of antibiotic resistance worldwide,” says Dr Marc Sprenger, director of WHO’s Antimicrobial Resistance Secretariat.
“Some of the world’s most common – and potentially most dangerous – infections are proving drug-resistant,” adds Sprenger. “And most worrying of all, pathogens don’t respect national borders. That’s why WHO is encouraging all countries to set up good surveillance systems for detecting drug resistance that can provide data to this global system.”
To date, 52 countries (25 high-income, 20 middle-income and 7 low-income countries) are enrolled in WHO’s Global Antimicrobial Surveillance System. For the first report, 40 countries provided information about their national surveillance systems and 22 countries also provided data on levels of antibiotic resistance.
“The report is a vital first step towards improving our understanding of the extent of antimicrobial resistance. Surveillance is in its infancy, but it is vital to develop it if we are to anticipate and tackle one of the biggest threats to global public health,” says Dr Carmem Pessoa-Silva, who coordinates the new surveillance system at WHO.
Data presented in this first GLASS report vary widely in quality and completeness. Some countries face major challenges in building their national surveillance systems, including a lack of personnel, funds and infrastructure.
However, WHO is supporting more countries to set up national antimicrobial resistance surveillance systems that can produce reliable, meaningful data. GLASS is helping to standardize the way that countries collect data and enable a more complete picture about antimicrobial resistance patterns and trends.
Solid drug resistance surveillance programs in TB, HIV and malaria have been functioning for many years and have helped estimate disease burden, plan diagnostic and treatment services, monitor the effectiveness of control interventions, and design effective treatment regimens to address and prevent future resistance. GLASS is expected to perform a similar function for common bacterial pathogens.




Top Comments
Disclaimer & comment rulesCommenting for this story is now closed.
If you have a Facebook account, become a fan and comment on our Facebook Page!